Links #
Website Link: MO HealthNet (mymohealthportal.com)
Web Portal Link: MyMOHealthNet Member Portal (mymohealthportal.com)
Creating an Account #
- On the log in screen, the participant will need to select “Create one now” located at the bottom of the box in orange.
- When creating an account, the participant will need to use the Head of Household’s information.
- If the participant does not have this information, utilize available resources to help locate information for the participant. If you cannot locate information for the participant, they can call a choice counselor at 800-348-6627.
- Information needed for HOH: DCN, SSN, Birth Date
- Password:
- 10 characters long, uppercase letters, lowercase letters, one number (0-9), special characters (!,@,$%,*,etc.)
- Advise participant to write their password down and keep in a safe place for future use.
- Once all information is filled out the participant has the option to select paperless billing at the bottom of the page, before selecting the blue “create account” button.
- Make sure the participant understands this means that instead of getting their information through the mail it will go to the email address they supplied. Just let them know it is optional and if they feel the email supplied is not easily accessible, they do not have to select paperless billing.
- Participant should review all information to make sure it is correct, then select the blue “create account” button.
Log In: #
- To log in to the portal, the participant will need to enter their email address and password they used when they created their account.
- If the participants are having trouble with being locked out of their account, they can call a choice counselor at 800-348-6627
My Member Page: #
- This page will show all the members on the case.
- If the participant clicks on one of the member names, if will drop down information specific to this participant including name, DCN, Address, type of program/plan they have and phone number.
My Enrollment: #
- This page includes Opt-Out Request, Just Cause Transfer, Disenrollment Request, Third Party Liability, PCP Update, and Health Risk Assessment.
- Opt Out Request
- Select Opt Out Request, then they will need to select the participant they are wanting to request the opt out for.
- Once they select the participant, they will be given a list of reasons for opting out:
- Eligible for Supplemental Security Income (SSI)
- Participant with special health care needs and individuals with medical necessity
- Participant is disabled and 18 or younger
- Nursing Home
- Other
- Once the reason is selected, they will click “Finish”.
- A task will then be sent over to MHD and be researched before approving or denying the request.
- Just Cause Transfer
- Select Just Cause Transfer, then they will need to select the participant they are wanting to do the JCT on.
- Once they select the participant, they will be given a list of reasons for the JCT:
- Appeals/Hearings
- Grievances
- Moral and Religious Reasons
- Sanctions placed on a Health Plan for not following contract requirements.
- Participant of child’s provider is with a different health plan.
- AHS or state agency makes a mistake during a previous assignment process.
- The Participant would like the whole family on the same health plan.
- Provider is culturally insensitive.
- Poor quality of care
- No covered services or providers in your area who are skilled in dealing with your health care needs.
- The name, phone number, DOB, and DCN will auto populate, and they will need to fill in a brief description for reason.
- Once all steps are complete, participant will select “finish” and this will send a task to MHD to be researched before approving or denying the request.
- Disenrollment Request
- Select the Disenrollment Request, then they will need to select the participant they are wanting to disenroll.
- Once they select the participant, they will choose a reason for disenrollment:
- Aged Out
- Death
- Incarceration
- Moved Out of State
- After they have chosen a reason, they will select “finish”. This will send a task over to MHD and they will research before approving or denying the request.
- Third Party Liability
- Select Third Party Liability, on this tab, participants can electronically fill out and submit a TPL Form.
- The participant can select the member they are entering the form for.
- Once they select the member, they will fill out the form with the policyholder’s name, policy number, and insurance company.
- The participant should review the information entered, then click “Finish” and the form will be saved to their account.
- Primary Care Physician (PCP) Update
- When this tab is chosen it will tell them to contact their Managed Care Health Plan to change their PCP.
- Health Risk Assessment
- Select Health Risk Assessment, then they will need to select the participant they would like to submit the HRA for.
- After selecting the participant, they will answer all questions on the form before selecting “finish”.
- The form will be uploaded straight to their account once complete.
- Opt Out Request
Provider Search: #
- When the participant clicks the Provider Search tab a “Search Provider” screen will come up.
- On this page, the participant can enter the provider type, health plan, specialty, provider name, zip code, distance, and zip code to find providers in their area.
- Once filters have been added the participant will select “search” and this will show them providers within the distance they chose from the zip code.
- The map will display red pins for each provider that was found based on the search filters. The participant can click on any of the pins and the information specific to that pin will show up on the right side of the map.
My Letters: #
- This tab gives the participant the ability to view and print letters that have been sent to them or e-notices they have.
- The participant will see the title of the notices/letters and date they were sent and can also search the notices at the top of the screen.
Message Us: #
- On this tab the participant can send secure messages to the enrollment broke about their Mo Healthnet.
- To send a message, the participant will click the blue plus sign. They will get a response within 2 business days.
- Any messages sent or replies that come in, will be save under this tab.
- To send a message, the participant will click the blue plus sign. They will get a response within 2 business days.
More Features: #
- When the participant selects this tab, a screen will come up with 3 additional tabs: My Documents, File a Complaint, and History.
- My Documents:
- When the participant clicks this tab, it will bring up all documents that have been uploaded into the portal.
- Participants can also upload a new document by clicking the blue file button on the right.
- After the participant clicks the blue file button a box will come up allowing them to choose the member they want to upload the document for.
- Once the member is selected, another box will come up letting the participant choose the type of document they are uploading.
- Last, a box will come up telling the client 3 steps to finish uploading the document: Give it a Name, choose your pages, sort and attach. The participant will need to follow the directions to finish the upload.
- File a Complaint:
- When the participant clicks this tab, it will ask you to select what member is filing the complaint.
- The next screen will ask the participant who the complaint is against with the options being: AHS, Mo Healthnet, Manage Health Plan.
- The participant will then complete the form and select finish to submit the complaint.
- History:
- The history section will show the participant a timeline of all activity on the account.
- Selecting the orange person icon at the top right corner will give the following options: Account Preferences, Language, Help, Log out.
- My Documents:
Premium Payment Online: #
Log In:
- To log in to the portal, the participant will need to enter their email address and password they used when they signed up.
My Member Page:
- After they have logged in, they will arrive at the “My Member Page”
- On the left side of the screen there will be a list of 7 tabs for the client to choose from. They will need to select the “Payment Details” tab, which is the second tab from the bottom of the list.
Payment Details:
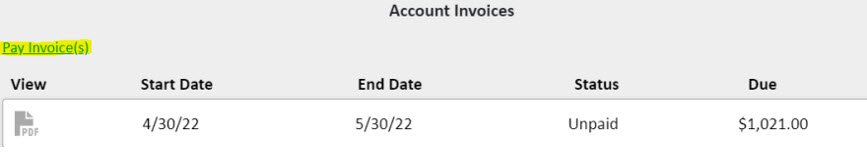
- On this page the participant can view their invoices and the status of the invoice.
- Invoice Status’: Paid, Unpaid, Past Due, Refunded
Paying an Invoice:
- To pay an invoice the client will select Pay Invoice(s) located under the Account invoices to the left.
- Once they select Pay Invoice(s), a box will come up with the list of invoices they can choose from to pay.
- The client will need to check the box next to the invoice they want to pay and click select.

-
- Make sure the client knows what month of coverage they are paying for with the invoice they select.
EX: The invoice below (which is also the invoice shown above in Section 2 Part A) would activate coverage for the month of 05/2022
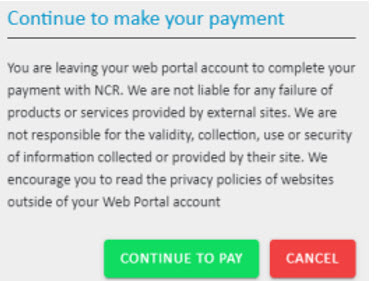
- After the client selects the invoice, a box will pop up stating the client will be redirected to complete their payment with NCR.
- Advise client to select the green “Continue to Pay” button:
- Payment Screen:
- The client will enter their information including their name. address, email, and phone number.
- Once their information has been entered, they will select the green “Next Step: Add Payment Method” button.
- Here they can select e-check or Credit Card depending on the payment method being used.
- The service fee for a Credit Card is 2.0%+0.25 cents on all amounts.
- The service fee for a e-check (routing and account number) is 0.50 cents for all amounts.
- Review Payment:
- Once the Payment Method has been entered the client can review the payment to make sure all information is correct, then select the green “Make Payment” button to complete the payment.
- If the client decides they want to cancel the payment, they can select “Cancel Transaction” to the right of the screen at any time and they will be redirected back to the web portal.
- Status Update:
- When paying by credit card, the web portal should update the invoiced status to show PAID immediately.
- When paying by e-check (bank account), it may take a day or two for the status to update to PAID.