Effective August 13, 2023, FAMIS allows Family Support Division (FSD) staff to:
-
- Send an Aged, Blind, and Disabled Supplement (FAABD) and Request for Information (FA-325) to any participant that has indicated that they are over the age of 65, blind, or disabled.
- Track if a supplement was returned (or information was obtained).
- Systematically reject the Non-MAGI application for failure to return the supplement information.
The FAABD form is a system-generated version of the Aged, Blind, and Disabled Supplement (IM-1ABDS). This allows staff to have the eligibility system print and mail the form. It also allows the case to pend and then reject if the supplement is not returned.
When to use the IM1-SSL or IM1-ABDS as Application Date #
- Use IM-1SSL date when:
- The IM-1ABDS is returned with the application, or while the application is pending a MAGI determination.
- The participant marks they are blind and are requesting cash benefits.
- The participant marks they are residing in a facility, s they may be eligible for SNC.
- The participant is not eligible for any MAGI programs.
- Use IM-1ABDS date when:
- The IM1-ABDS is received after the participant is found eligible for any MAGI program, as a change in circumstance.
- The IM1-ABDS is received within 90 days of the initial application being rejected for failure to complete the supplement, due to 90-day reconsideration period.
MHABD Supplement Information Screen #
Sending the form and tracking the supplement’s return (or if information was obtained) will take place on the MHABD Supplement Information (1ABDS/FM1L) screen.
Screen shows:
-
- SCN
- HOH DCN
- The question “Do you need to send a supplement?” a field for a response.
- A field to capture the date the FAABD was sent.
- A field to capture the date the supplement was returned, or information was provided.
The MHABD Supplement Information screen appears in CONFLOWS before the Eligibility Unit Member Role screen (EUMEMROL/FM3Z). You can also fastpath to the screen using 1ABDS or FM1L.
1ABDS Entries #
The first question on the screen captures if a supplement needs to be sent, if one has already been received, or if one has already been sent.
Do you need to send a supplement?
-
- Y = Yes. I need FAMIS to send a FAABD and a FA325 to the participant.
-
- Leave both date fields blank. FAMIS will fill the Date FAABD Sent field after it is generated and mailed, and you will be able to update the Date Supplement Received/Information Obtained field when it is returned.
- Note: This does not change the requirement to attempt to contact the participant and collect the information by phone before sending a request.
- Example: FSD staff registered a Non-MAGI application. There was not a supplement form provided with or after the application and the staff member was not able to reach the participant by phone.
-
- Y = Yes. I need FAMIS to send a FAABD and a FA325 to the participant.
-
- N = No. I do not need FAMIS to send a FAABD.
-
- Enter the Date Supplement Received/Information Obtained field before you can move forward. Capture the date the supplement was returned by the participant, or the date the information was obtained, such as during a Supplemental Nutrition Assistance Program (SNAP) interview or by the participant contacting the FSD Information Center.
- Example: FSD staff registered a Non-MAGI application. The supplement was provided the same day as the application.
- Example: FSD staff registered a Non-MAGI application and spoke to the participant by phone to collect all the necessary supplement information.
-
- N = No. I do not need FAMIS to send a FAABD.
-
- M = Manual. I already sent the participant a supplement form and a request for information with a due date.
-
- Enter the Date FAABD Sent field before you can move forward. Capture the date the supplement was sent to the participant.
- Example: FSD staff sent the participant a supplement while they were requesting other required verification while exploring MAGI coverage.
-
- M = Manual. I already sent the participant a supplement form and a request for information with a due date.
Note: FSD staff cannot generate a FAABD from DOCQUE. If a supplement is not sent when the application is registered, but it is later discovered that one needs to be sent for a pending application, staff can send one by fastpathing to 1ABDS/FM1L, changing the “Do you need to send a supplement?” field to Y, and clearing date from the other fields.
If a Y entry is entered on the first question, the system sends an FAABD and a FA325. Staff are to generate and edit the FA325.
-
- Fastpath to the OUTVERF screen and generate the FA-325. Edit the text fields on the FA-325, See FA-325 text for FA-ABD below.
- Edited FA-325 & FA-ABD in FAMIS will need to be printed and mailed to the participant.
- NOTE: FA-ABD will generate and be sent out in the overnight batch process. Staff will have to wait till the next day to print and mail if needed. Follow your local office procedure for mail-outs.
- FA-325 text for FA-ABD:
YOU ARE GETTING THIS REQUEST BECAUSE YOU APPLIED FOR MO HEALTHNET AND SAID YOU ARE DISABLED OR OVER THE AGE OF 65. YOU MAY HAVE RECEIVED A NOTICE THAT YOU ARE NOT ELIGIBLE FOR MOHEALTHNET. THAT LETTER WAS FOR THE ADULT EXPANSION GROUP AND FAMILY MO HEALTHNET PROGRAMS.
FILL OUT THE ENCLOSED AGED, BLIND, AND DISABLED SUPPLEMENT FORM AND RETURN IT TO US. IF YOU DO NOT RETURN THIS FORM, YOUR MO HEALTHNET FOR THE AGED, BLIND, AND DISABLED APPLICATION WILL BE REJECTED.
PLEASE UPLOAD AT MYDSSUPLOAD.MO.GOV, FAX TO 573-526-9400, OR MAIL TO THE ADDRESS SHOWN ABOVE. LIST YOUR NAME, DATE OF BIRTH & SOCIAL SECURITY OR DCN ON ALL PAGES OF ANY DOCUMENTS YOU SEND TO US.
After staff update the 1ABDS screen, staff must make the appropriate application registration comment, including their entries on the 1ABDS screen.
The application should remain at the beginning of the controlled flow (CONFLOWS) until the supplement information is returned.
Supplement Received with no Application or Pending Application (No active coverage) #
When a supplement is received with no IM-1SSL, and the participant does not have active MAGI or Non-MAGI OR any pending applications.
Staff should:
- Check the ECM for any additional documentation that could have been uploaded with a current address. If there are no other documents with a current address in the ECM, verify the participants address with MODL.
- Mail a IM-1SSL to the participant.
- Make a comment regarding actions taken.
- MEDES: If the participant is known to MEDES, you can comment on the “Person Page” then “Client Contact”
- FAMIS: If there is a prior closed case for the participant, you can comment on “EUMEMROL”
- The IM-1ABDS should be used if it was provided in the month of application, or in one of the prior quarter months once an application is received.
- EX: An IM-1ABDS was received April 2025, but there was no active case or pending application. As long as an application is received prior to July 31,2025, a new IM-1ABDS is not required, unless information is questionable.
Supplement Received as Verification #
When the supplement is returned, or when the information is obtained, FSD staff must update the 1ABDS screen to capture the “Date Supplement Returned/Information Obtained.”
Staff should:
-
- Fastpath to 1ABDS screen.
- Add the date that the information was returned.
- Complete CONFLOWS with the information provided.
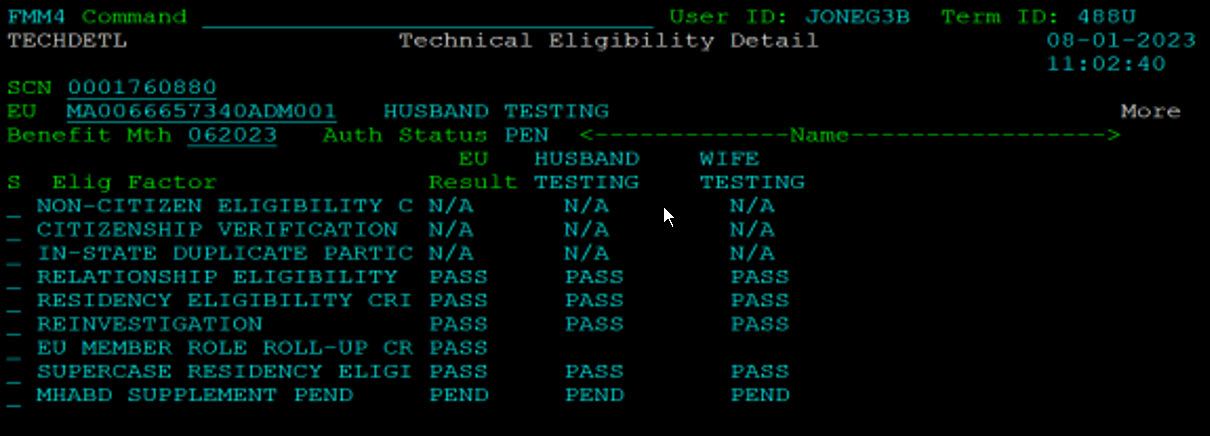
If there is no date entered, the application will PEND for MHABD SUPPLEMENT PEND on the Technical Eligibility Detail screen (TECHDETL/FMM4).
-
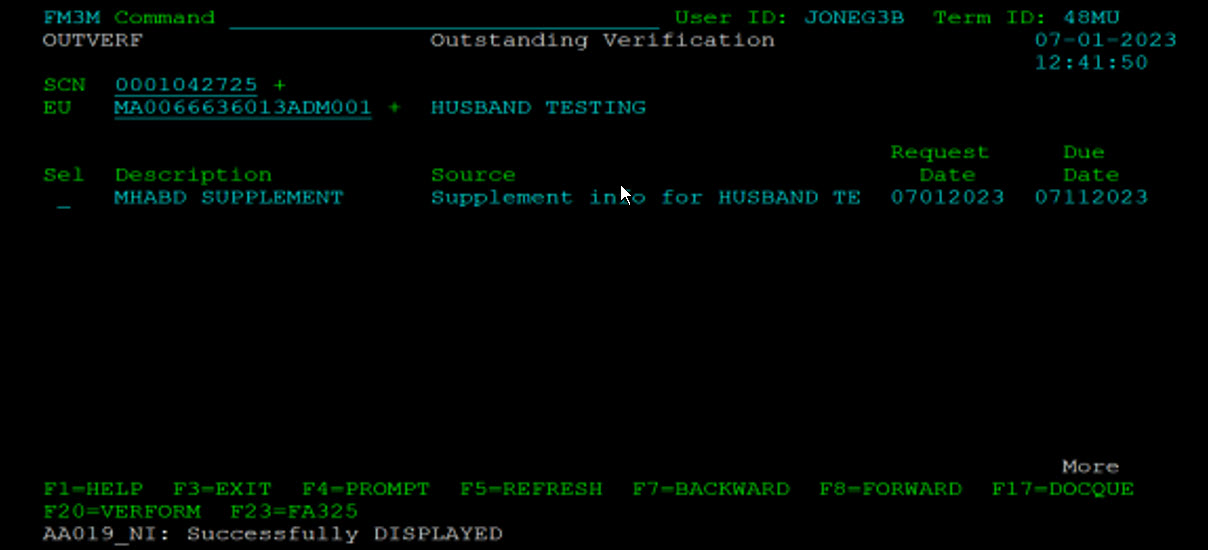
- The application will continue to pend and show on outstanding verification (OUTVERF/FM3M) until a date is entered on “Date Supplement Returned/Information Obtained” on the 1ABDS screen.
EXP: FAMIS screen Technical Eligibility Detail. Screen shows eligibility details for applicant Husband Testing. The last row shows the MHABD Supplement PEND factor. The EU, Husband Testing, and Wife Testing all show a PEND result.
Supplement Received as Change in Circumstance #
-
- When a supplement is received, and the participant has active Non-MAGI, staff should:
-
- Treat the supplement as a change in circumstance
- Follow the Change in Circumstances in FAMIS guide to enter all new or changed information into FAMIS and evaluate the impact on eligibility.
-
- When a supplement is received, and the participant has active MAGI, staff should:
-
- Treat the supplement as a change in circumstance to explore Non-MAGI.
- Register the Non-MAGI application with the date of the IM-1ABDS was received.
- All information in MEDES and electronic resources should be used to complete the CiC as an ex parte review to process in FAMIS. Do not re-verify or request information if it is still current.
-
- When a supplement is received, and the participant has active Non-MAGI, staff should:
Supplement Not Returned Timely #
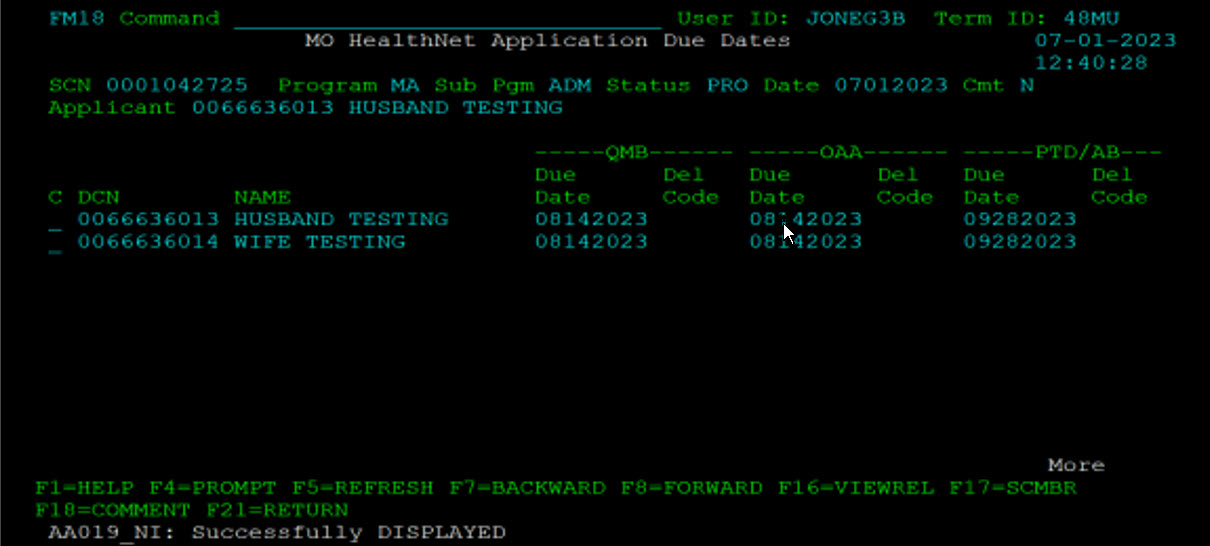
If the information is not returned AND a date is not entered on 1ABDS screen, FAMIS will reject the application 45 days after the application request date, or after the outstanding verification due date, whichever is the later date.
-
- EXP: FAMIS screen showing MO HealthNet Application Due Dates. Husband and Wife participants are shown with due dates for MO HealthNet categories.
-
- EXP: FAMIS screen showing Outstanding Verification. MHABD Supplement, Supplement info for Husband with a request date and a due date
Both the notice sent to the participant and the eligibility system will display the rejection reason, FSI:
-
- Notice
-
- FSI – Supplemental information was requested to determine eligibility and was not provided (42 CFR 435.911, RSMo 208.010, RSMo 208.210)
-
- FAMIS
-
- FSI – Failure to provide supplemental information.
-
- Notice
If the application is rejected and the IM-1ABDS is later provided, FSD staff must review application timeframes and follow current Cancel Reject/Cancel Close in FAMIS.
-
- If it is required to re-register the application, the registration date will be the date the IM1-ABDS was received.