Tools #
Guidance #
FSD team members have ten days after learning about a change to determine if any additional verification/information is needed and to request it from the EU.
Non-MAGI:
- Non-MAGI households must report changes affecting eligibility factors within ten (10) calendar days of the change. When the change is obtaining employment or a change in rate of pay, the change date is the date of the first paycheck or first paycheck with the changed rate of pay.
- Enter all new or changed information into FAMIS and evaluate the impact on eligibility
-
- If the change is reported timely and would result in increased coverage or a better benefit, the change is effective the month of the report.
- If the change is not reported within ten calendar days and would result in an increase in coverage, the change is effective the month of report, not the month in which the change occurred.
- If the change results in eligibility for more than one Non-MAGI coverage (such as Spend Down to TWHA or SLMB2), decisions regarding coverage must be made by the participant or the Authorized Rep. If the participant requests to be switched to the other program, do not require a new application and complete an eligibility determination as an ex parte (which means without contacting the participant).
- If the action results in decreased coverage (including increase in Spend Down), an Advanced Notice of Adverse Action is required and the change becomes effective no later than the month following the month the change is reported unless an invoice has already been sent for the following month. In that case, the change becomes effective the second month. Example: If a participant’s income increases 10/10, Adverse Action expires 10/20, the November invoice would have been sent out on 10/1. Therefore, the increase in Spend Down is not affected until December with the new invoice and new Spend Down amount.
- If the action results in no longer meeting eligibility, explore eligibility MAGI and AEG in MEDES. Register a MAGI application in MEDES using the most recent information from the participant’s Non-MAGI case and process to determine eligibility.
-
SNAP:
- SNAP households are required to report certain changes by the tenth day of the month, following the month in which the change occurred.
- The only changes which are required to be reported are:
-
-
- Gross monthly income exceeds 130% of poverty
- Reduction in the number of hours worked by ABAWD individuals
- Lottery or gambling winnings equal to or greater than the current resource limit for elderly/disabled households or more in a single game.
- Note: See 13.5.8 SNAP Lottery and Gambling Winnings for additional information.
-
- During a certification period, changes may be reported by the household, an outside source or an automated report. Even if information is verified upon receipt, it can still be considered unclear if additional verification/information is needed to act on the change.
- The agency must request clarification and/or verification (if applicable) of reported changes in household circumstances for unclear information if the information is:
-
- Information is less than 60 days old from the date of receipt and is required to be reported by the household, or
- Significantly conflicting with information reported at the time of application and approved certification, enough to bring the household’s eligibility into question, or
- A match with a participant data matching system is received
-
- Note: This information must be handled differently from other unclear information. Refer to 13.2 Information from Certain Data Matches in the FSD Policy Manual
-
-
TA:
- Temporary Assistance participants must report changes in circumstances within ten (10) days.
- Enter all new or changed information into FAMIS and evaluate the impact on eligibility.
-
- Any grant decrease becomes effective the month following the month of change or the month following expiration of the notice of adverse action.
- Any grant increase becomes effective no later than the month following the month the change is reported.
- When monthly income decreases by $50 or more, a deficiency payment is made for the month in which the change is reported.
-
Step 1: Fastpath to all applicable screens to complete the change #
See FAMIS Fastpath Reference List for assistance in locating screen fastpaths.
Address Change #
Screen Help
![]() FAMIS Participant Search/PRSNSRCH
FAMIS Participant Search/PRSNSRCH
Guidance
-
- The residential (physical) address must be a valid Missouri address. (FAMIS organizes applications and cases by residential address. Exceptions to using the residential address on SCMBR are: Safe At Home and a Post Office Box when the residential address is a battered women’s shelter.)
-
- Note: SNAP: When a new address is reported, contact the household by phone to obtain the new shelter expense information. If expenses have changed, end date the existing expenses for the prior month, add the new expenses current month with CS as the verification code and authorize the new case actions. If telephone contact is unsuccessful, complete the same steps as stated above except entering $0 in the amount field and leave the verification code blank. Pend the case for shelter expenses and send an FA-325 to request the updated shelter expense amounts.
-
- The participant must reside in Missouri with the intent to remain in the state. Residents in certain public institutions are not eligible on this factor.
-
- Note: SNAP: Intent to remain in the state is NOT required
- Note: Vendor:
-
- For single individuals who live in a nursing facility, the residential address is that of the nursing facility with living arrangement code ‘Nursing Home’ (NH).
- For a married couple when one spouse is institutionalized, the address of the community spouse is the residential address (Living Arrangement type RA.) The nursing home address is captured on the Facility and Placement Information Details screen.
- For a married couple when both reside in the same institution, and for single individuals, the facility address is the residential address and the living arrangement type ‘Nursing Home/Residential Care’ (NH) is used.
- For a married couple with spouses residing in separate institutions, the address of the FSD county office where the couple originally resided is used as the residential address with a living arrangement type ‘Nursing Home/Residential Care’ (NH). Each spouse’s facility address is captured on the Person Detail screen, so that they may receive correspondence.
- The Authorized Representative’s mailing address is captured on the Representative Detail screen. The case remains in the claimant(s)’ county of residence even when the Authorized Representative’s address is in another county.
-
-
- The applicant’s declaration of residency is discussed later during the controlled flow of the application process and is entered on the RESIDENT screen.
-
- Note: SNAP: Enter the verification code on Application Detail (FM13) and document the verification by adding a comment to the Food Stamp Eligibility Unit Member Role (EUMEMROL/FM3Z) screen.
-
- The residential (physical) address must be a valid Missouri address. (FAMIS organizes applications and cases by residential address. Exceptions to using the residential address on SCMBR are: Safe At Home and a Post Office Box when the residential address is a battered women’s shelter.)
Address Change
Question 1: Does the address change apply to all members of the household?
-
-
-
- If no, first see Removing a Deceased Supercase/Eligibility Unit Member
- If yes, continue to next question
-
-
Question 2: Is the new address a Safe At Home address?
-
-
-
- If yes, see Safe at Home – Protected Caseloads User Guide
- If no, continue to next question
-
-
Question 3: If the participant homeless?
-
-
-
- If yes, see Homeless ADRES Flow Chart
-
- Homeless participants must have a mailing address. If participant marked homeless, even if a physical address is reported, enter homeless as the physical address with HL as the living arrangements and enter the mailing address on the Person Detail screen (PRSNDTL) per the Homeless ADRES Flow Chart.
-
- If no, see ADRES Flow Chart
- If yes, see Homeless ADRES Flow Chart
-
-
Question 4: Having trouble getting the address to clear on SCMBR?
-
-
-
- If yes, see CD1P: Code 1 Plus Guide
-
-
Update Address in MEDES
-
- After changing an address in FAMIS, see Address Change on an Integrated Case/CIC guide to confirm correct address is reflected in MEDES
Bad Address
Question 1: Was returned mail received from the participant?
-
-
-
- If yes, see Returned Mail ADRES Guide
-
-
Question 2: Were you taken to ADRES while trying to register an application?
-
-
-
- If yes, see How to Resolve Bad Address on ADRES
-
-
Mailing Address
Question 1: Does the mailing address need to be removed?
-
-
-
- If yes, see Deleting a Person Mailing Address on ADRES
-
-
Verification
Follow FCR steps to verify.
- Can we get it?
-
- MODL
- IMES
- IIVE
- LIHEAP
-
- If customer needs to provide verification, common verifications are:
-
- Unexpired driver’s license with current address
- Rent or mortgage receipts
- Lease
- Utility bills
- Any mail with current address
-
Comment
Comment on program specific EUMEMROL/FM3Z when a new address is reported and entered into FAMIS
-
- The name of the person who reported the new address
- The date and how the address was reported
- The new address
- How the address was verified, if it was
- SNAP: Obtain new shelter expense information or request it if not initially provided and the participant cannot be reached by phone
MHABD couple cases, record on MHABD EUMEMROL/FM3Z who lives where, by name, when there is a community spouse and an institutionalized spouse
Adding/Removing Person from Supercase/EU #
Screen Help
Question 1: Does the person need to be added to the Supercase or EU?
-
- If yes, see Application and Add-A-Person Registration Guide
- If no, continue to next question
Question 2: Is the person to be removed deceased?
-
- If yes, see Removing a Deceased Supercase/Eligibility Unit Member
-
- During an MHABD application or annual review, access the AfGE portal if additional information is needed to confirm if the participant/applicant is deceased or incarcerated.
-
- If no, continue to next question
- If yes, see Removing a Deceased Supercase/Eligibility Unit Member
Question 3: Is the person to be removed the Head of Household of the EU?
-
- If yes, do not remove the person and search ADRES in FAMIS Resources
- If no, continue to the next question
Question 4: Is the person to be removed a member of the same EU of the person reporting the change?
-
- If yes, see Removing a Supercase or Eligibility Unit Member
- If no, do not remove the person until confirming the action with your supervisor. Then reference Removing a Supercase or Eligibility Unit Member for the participant who DOES NOT have an active case in FAMIS
Verification
-
- Accept CS unless questionable, however;
- CC- for whom Temporary Assistance has been requested. This is due to current FAMIS functionality. TA policy states CS is acceptable unless questionable.
- GS- Accurint Statement – Accurint for Government Eligibility information is used and additional information or verification is needed. GS will prompt FA325 to be generated.
- GC- Accurint Confirmation – Uses GC if no additional verification is needed after accessing Accurint for Government Eligibility or updates GS to GC after the additional information or verification is received from the participant
Comment
Comment on program specific EUMEMROL/FM3Z when adding/removing persons to existing Supercase and household/EUs
-
- Identify by name, the person who is adding or removing another participant
- Record your decisions:
-
- If not being added to a household/EU, explain why based on policy
- If being adding to a household/EU
-
- Record if they wanted to be added, and if not why the person is mandatory per policy for that program
-
-
End Dating Resource for Non-MAGI (Excluding Vendor/Supplemental Nursing Care) #
-
- When a participant declares that a resource no longer exists, staff should accept the participant’s statement without requiring further verification if:
-
- The resource in conjunction with other known or declared resources does not create ineligibility if included and
- The termination of the resource is reasonable.
- NOTE: If the termination of the resource is outside of the application timeframe (including prior quarter) or outside of the reinvestigation timeframe, it should be considered as reasonable unless there are extenuating circumstances. Such circumstances should be reviewed by a supervisor prior to requesting verification from the participant.
-
- When a participant declares that a resource no longer exists, staff should accept the participant’s statement without requiring further verification if:
-
- If these criteria are met, staff should end date the resource with the date that the Agency became aware of the termination, such as the date the reinvestigation form was received, or the date of the actual termination, if known.
-
- A comment should be added at the particular resource SELFRES stating that the participant is no longer declaring the resource and that the end of the resource is not in question.
-
- If the end of the resource is in question or would create eligibility issues, staff should first attempt to clarify the situation by following up with the participant via telephone. If unable to clarify in this manner, follow verification procedures in 10.2 Determining Countable Resources.
End Dating SMI Premium on MEDEXP Due to QMB/SLMB approval #
-
- Fastpath to FM0D/FAMISPAR, select the active Non-MAGI(MA) case and fastpath to FM4L/MEDHIST to check for QMB/SLMB coverage.
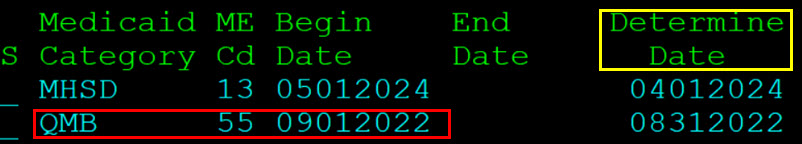
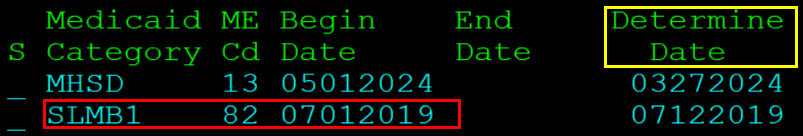
- MEDHIST verifies that participant has active QMB/SLMB. Below are examples of what MEDHIST will show if the participant has QMB or SLMB:
-
- QMB
-
- SLMB
-
- QMB
-
- Fastpath to MEDEXP:
-
- End date the Medicare Part A (PA) and/or Medicare Part B (SM) expense effective the month the QMB/SLMB benefits were approved (determination date).
- DO NOT wait for the Buy-In unit to start paying the SMI premium before ending the SMI expense for participants.
-
- Once the expenses have an end date, EDRES the case.
-
- While completing EDRES, note if the adjustment results in the case becoming a Spend Down or an increase to the Spend Down amount. If so, you will fastpath to MEDEXP and update the Spenddown amount effective the first month the change is reflected on EDRES.
-
- Comment on MEDEXP and EUMEMROL that PA/SM expense was ended and if there was a Spend Down expense that was added/updated.
Incarceration for MO HealthNet Participants #
Guidance
People who are incarcerated have a unique eligibility situation.
FAMIS generates a Notice of Match Results (NOMR/FA-601) for possible incarcerated participants during the controlled flow.
Note: Staff must review available electronic sources for prisoner information at application and recertification. On IIVE (SVES-Wire Third Party Query Response), a message will appear on the bottom, right-hand corner of the screen if prisoner information is available.
Question 1: Is the individual actively receiving healthcare coverage and is being reported as incarcerated?
-
- Yes, follow directions in 3.19.2 Suspending MO HealthNet Policy.
- No, go to Question 2
Question 2: Is the individual incarcerated, expected to be released within 60 days and requests MHN Application?
-
- Yes, follow direction in 3.19.9 Redetermination and Restoring Benefits After Release Policy.
- No, go to Question 3
Question 3: Is the Individual incarcerated and is admitted as inpatient stay for 24 hours or more at a medical facility outside of the Department of Corrections?
-
- Yes, follow directions in 3.19.8 Inpatient Services while Incarcerated Policy.
Step 2: Complete EDRES #
After changes are made, complete a new Eligibility Determination Resolution following Authorizing an Action guide.
Step 3: Request Verification #
Evaluate the specific change to determine appropriate verification needed (if applicable). Request verification via FA-325 or IM-31A allowing participants 10 days to comply.
Step 4: Comment #
- Customer's name
- Contact method (phone call to FSD, walk in, etc.)
- Contact date
- Summarize all application and/or case actions taken, authorized or voided
- Any information which was added, updated, or changed
- If the call was transferred, why and to which office, tier or person
- Date and detailed explanation of the reason, such as a list of the requested verification which was not provided
- Outcome of the worker initiated action